Streamlining the Credentialing & Enrollment Process for Healthcare Providers
- Hospitals
- Solo Practitioners
- Group Practices
- Medical Laboratories
- Skilled Nursing Facilities
- Home Health Agencies

Credentialing & Enrollment: A Vital Process for Healthcare Providers
Credentialing and enrollment are two essential processes in the healthcare industry that ensure providers meet regulatory standards and can receive reimbursement from insurance companies. These processes help maintain the quality of care, ensure compliance with industry regulations, and facilitate seamless billing and payment cycles.
What is Credentialing?
Credentialing is the process of verifying a healthcare provider’s qualifications, including education, training, licensure, certifications, work history, and background. This ensures that providers meet the necessary standards to practice medicine and deliver quality patient care.


The Credentialing Process:
-
Application Submission:
The provider submits credentials, licenses, and other required documents.
-
Primary Source Verification:
Educational institutions, licensing boards, and employers verify the information.
-
Background Checks:
Includes criminal history, malpractice claims, and disciplinary actions.
-
Committee Review & Approval:
A credentialing committee reviews the documents and grants approval.
-
Re-Credentialing:
Providers must renew their credentials periodically to maintain compliance.
Why is Credentialing Important?
- Ensures Patient Safety: Only qualified professionals are authorized to provide care.
- Regulatory Compliance: Meets accreditation and legal requirements.
- Reduces Medical Errors: Verifies providers’ expertise and experience.
- Builds Trust: Patients feel more secure knowing their providers are properly credentialed.
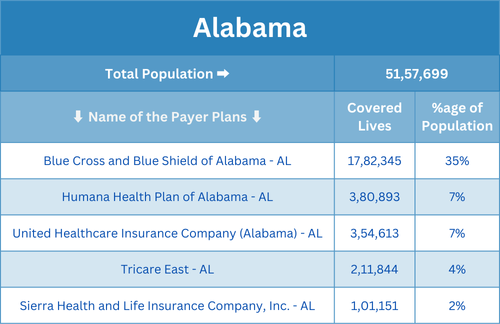
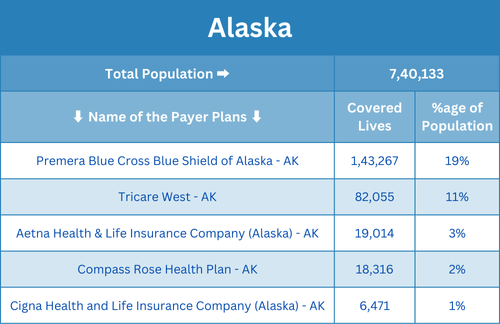
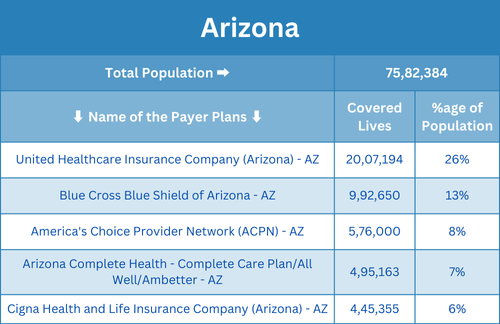
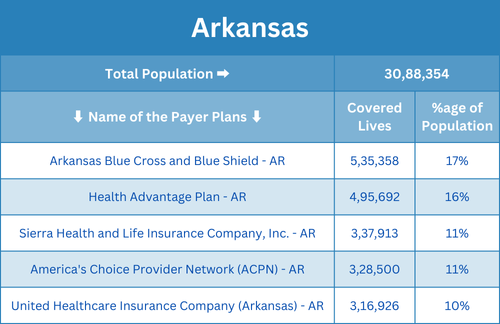
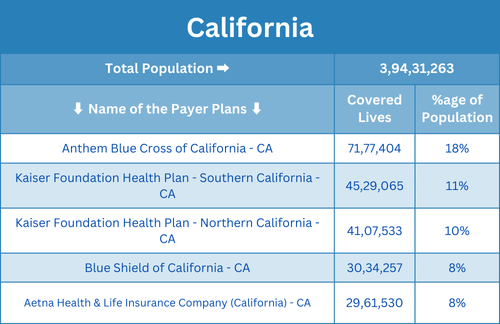
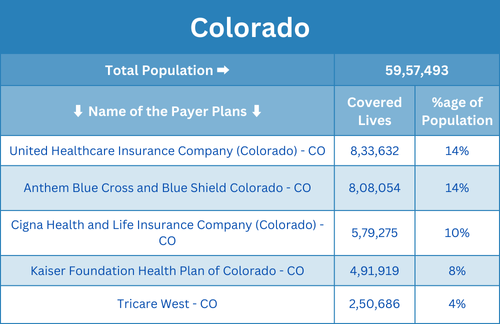
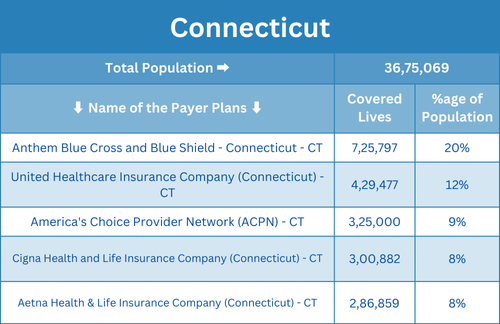
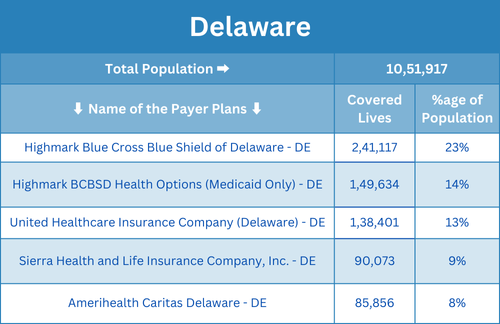
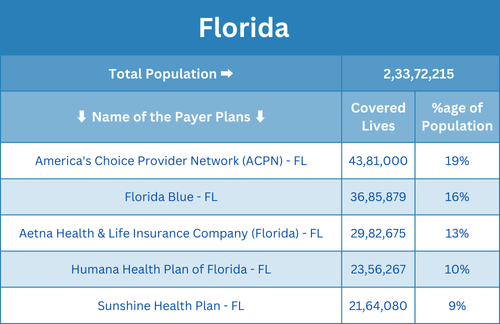
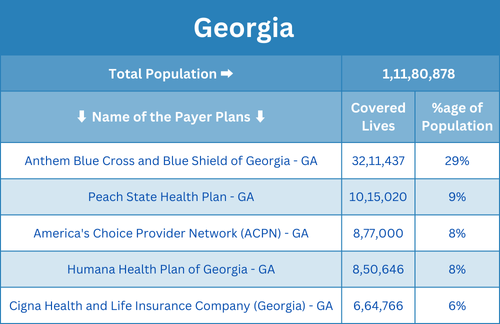
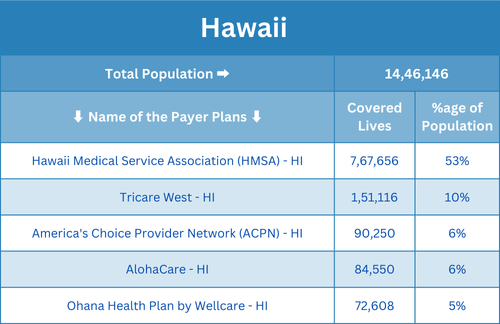
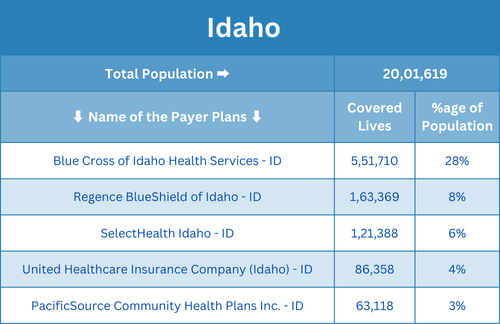
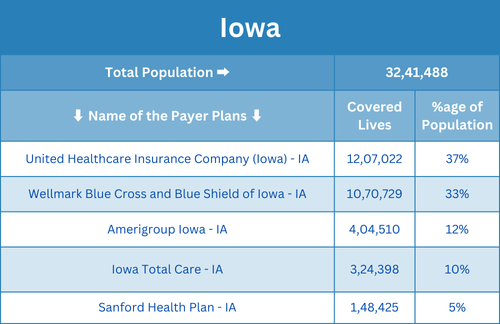
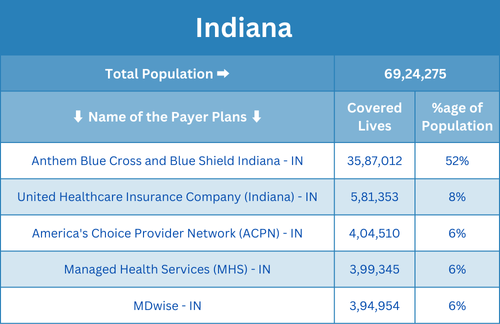
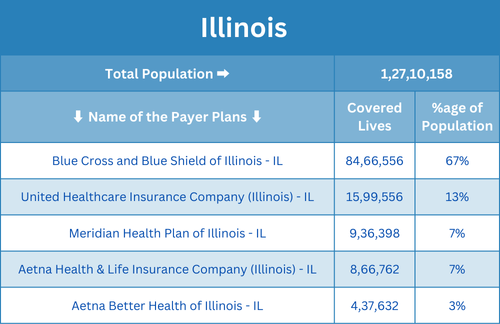
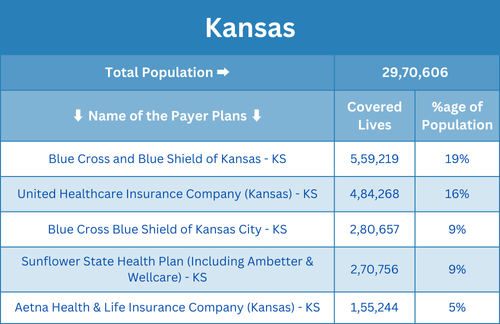
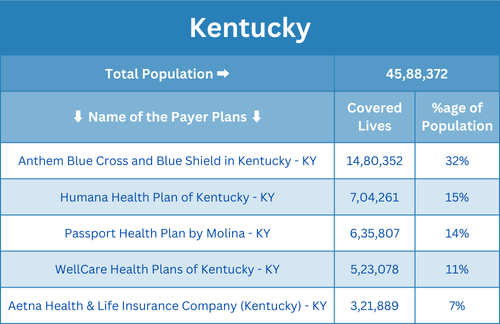
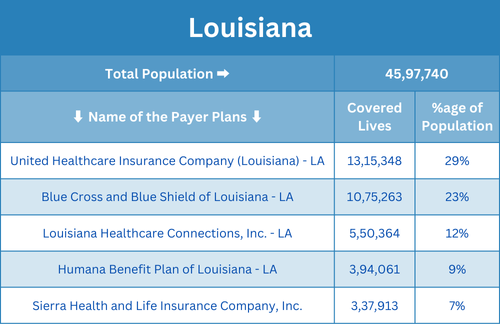
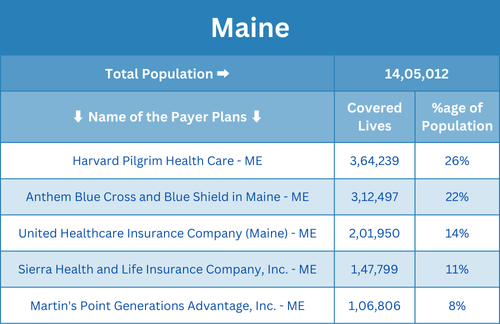
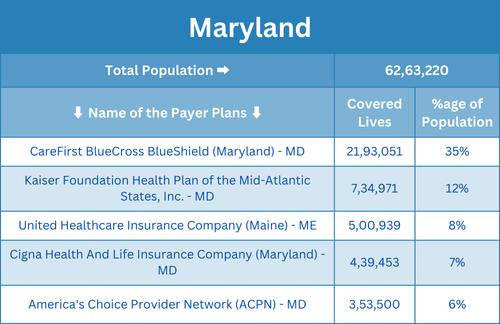
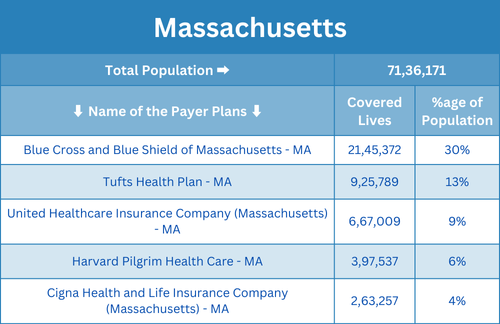
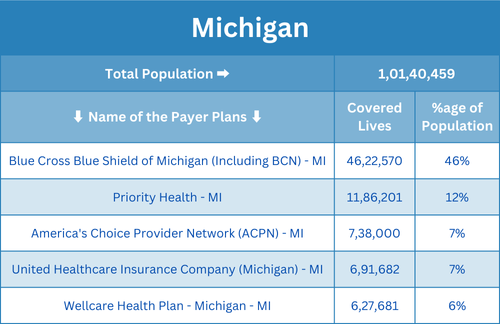
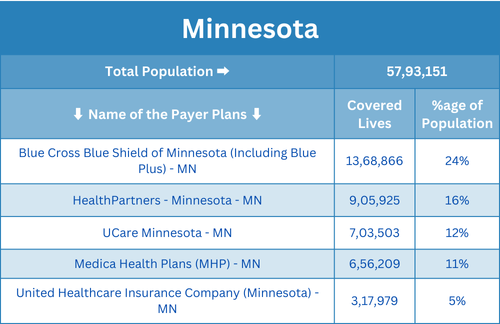
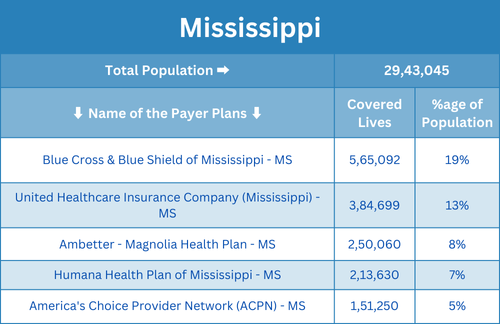
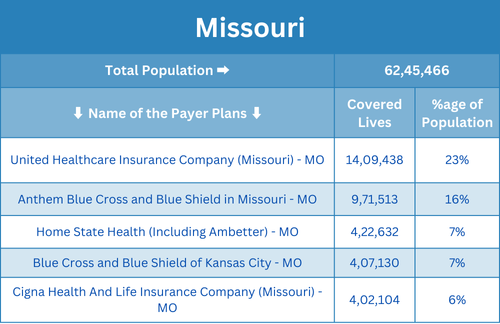
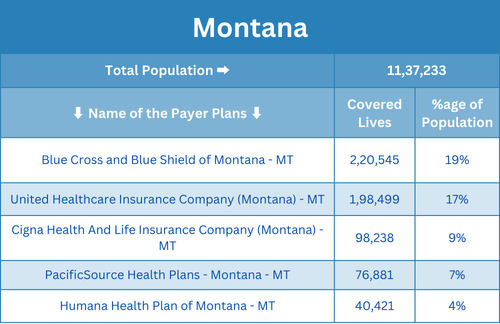
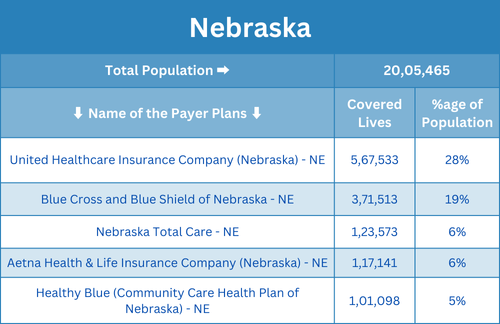
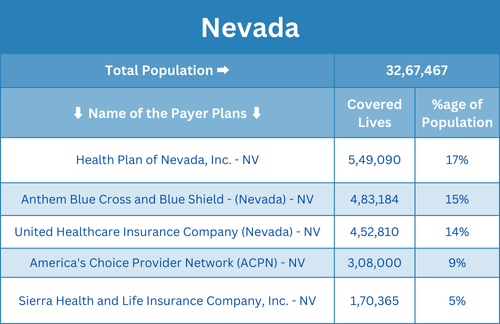
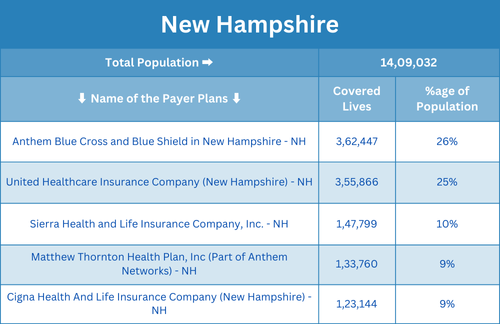
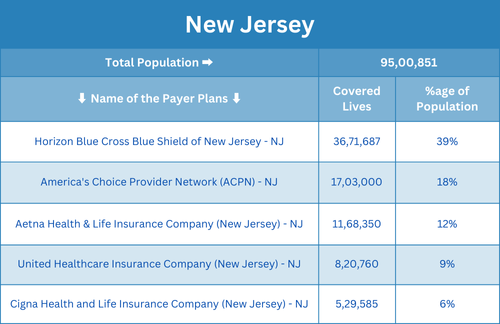
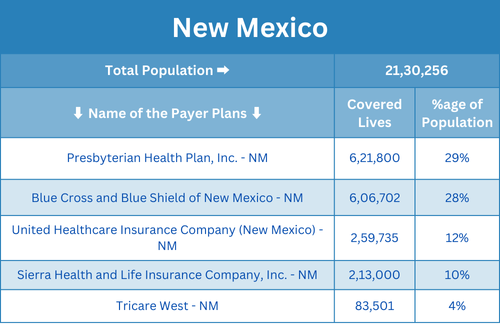
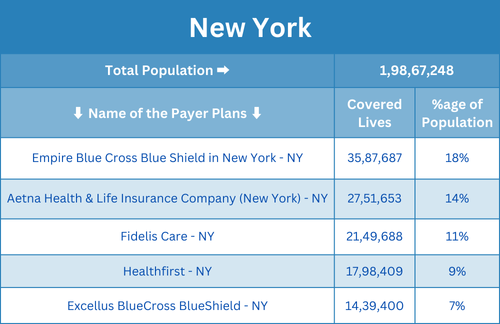
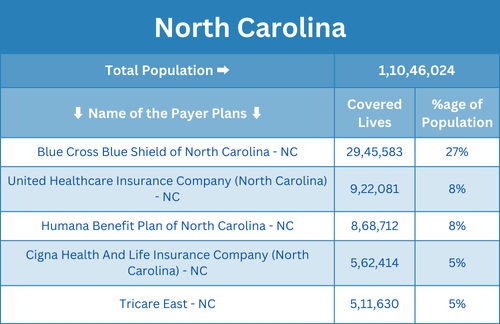
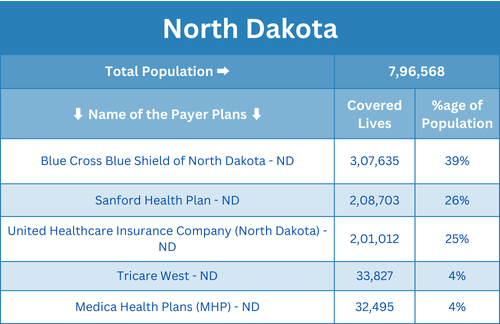
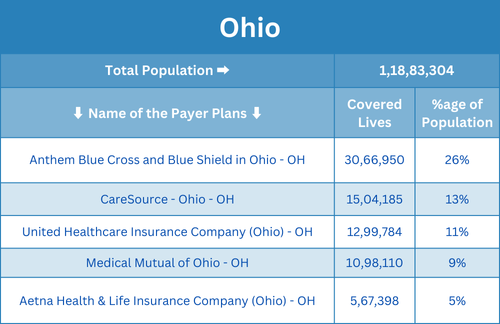
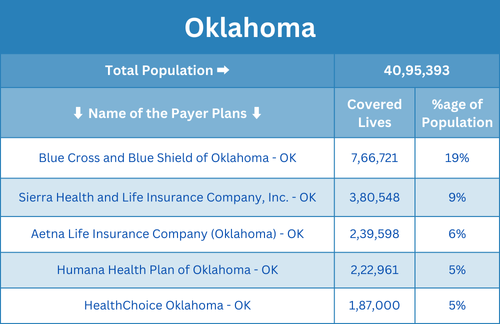
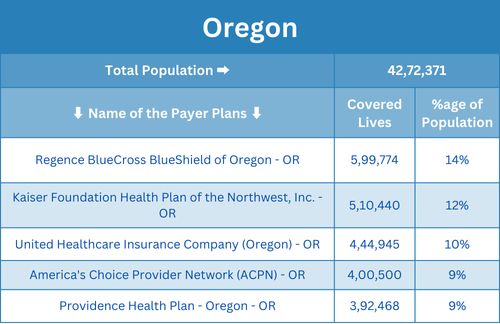
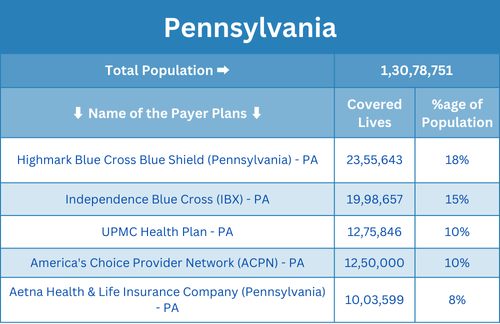
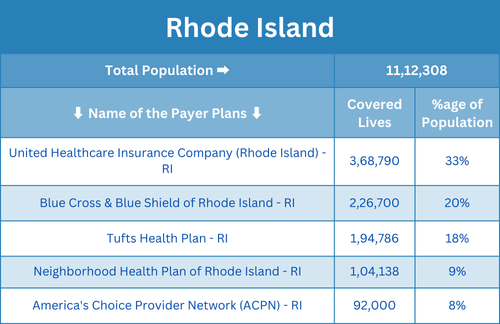
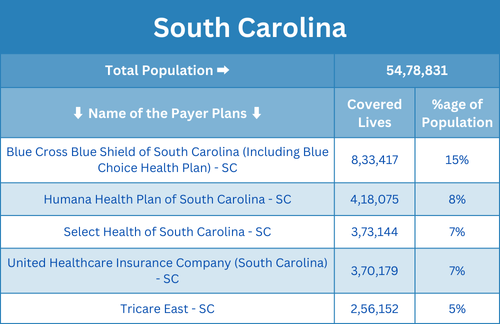
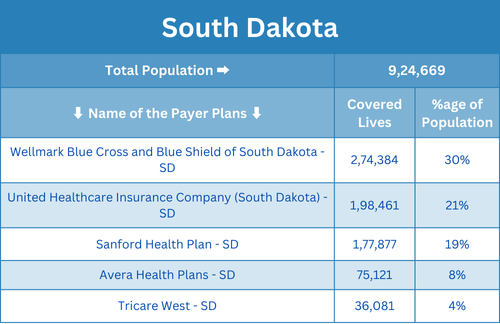
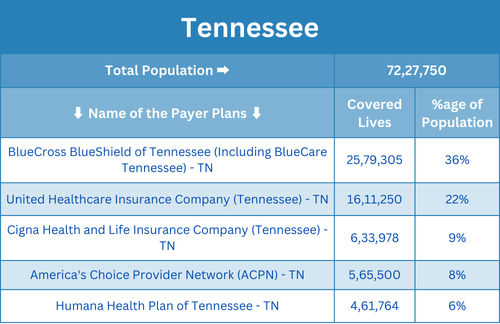
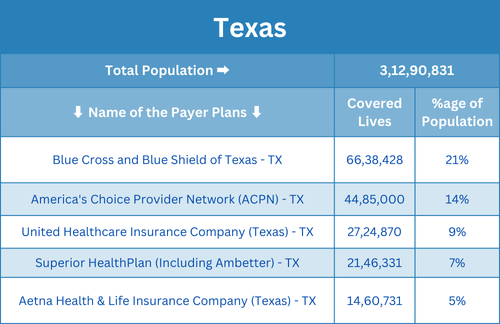
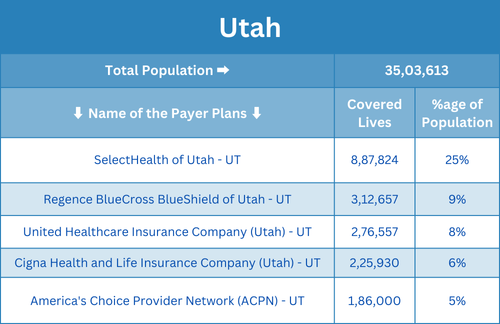
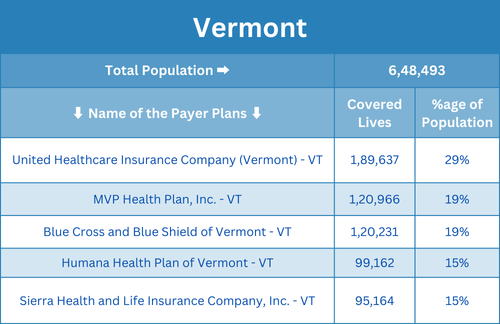
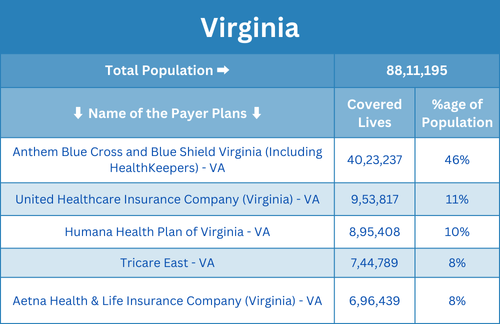
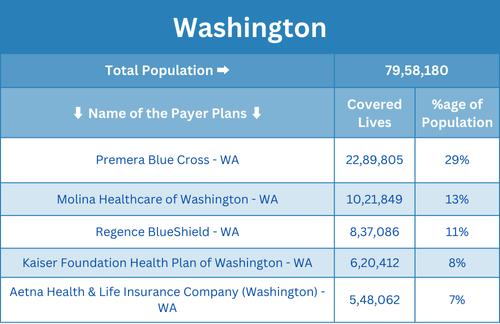
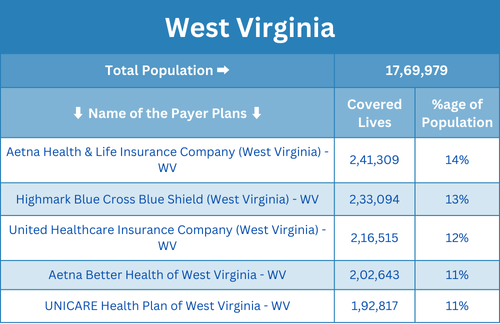
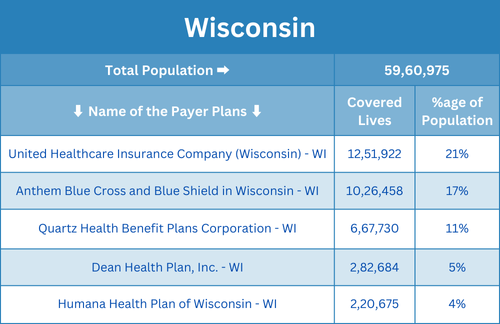
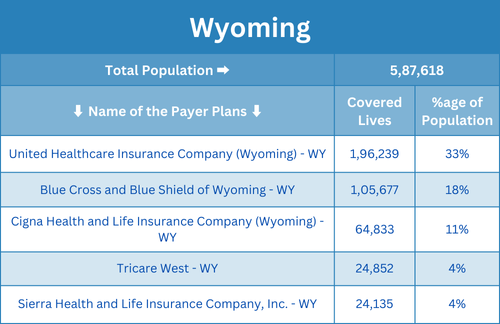
Disclaimer: Coverage data represents approximate figures compiled from various public sources and may not reflect current exact enrollment numbers.
What is Enrollment?
Provider enrollment is the process of getting healthcare providers registered with insurance networks, including private insurers, Medicare, and Medicaid, allowing them to bill and receive payment for services rendered.


The Enrollment Process:
-
Submit an Application:
Providers submit an enrollment application with necessary documentation.
-
Credential Verification:
Insurers review and verify the provider’s qualifications.
-
Approval & Contracting:
Once verified, the provider enters into a contract with the insurance company.
-
Billing Activation:
The provider can now submit claims and receive reimbursements.
Why is Enrollment Necessary?
- Enables Providers to Receive Reimbursements from insurance companies.
- Reduces Claim Denials by ensuring proper registration with payers.
- Improves Patient Access to Care as enrolled providers can serve insured patients.
- Supports Financial Stability for healthcare organizations by ensuring steady revenue flow.
What is Insurance Credentialing?
Insurance credentialing is the process by which healthcare providers become approved to participate in insurance networks, allowing them to bill insurance companies and receive reimbursements for the services they provide to insured patients. This process involves verifying a provider’s qualifications, including education, training, licenses, certifications, and work history, to ensure they meet the standards set by insurance payers, including Medicare, Medicaid, and private insurance companies.
The Insurance Credentialing Process
- Application Submission – Providers submit necessary documentation to insurance companies.
- Primary Source Verification (PSV) – Insurance payers verify the provider’s education, training, licensure, and work history.
- Background Checks – Includes malpractice claims, disciplinary actions, and legal compliance reviews.
- Approval & Contracting – Once verified, the provider signs a contract with the insurance company.
- Enrollment Activation – The provider is officially added to the insurer’s network and can begin billing.


Phases of Insurance Credentialing
The insurance credentialing process typically consists of three main phases:
1. Application & Documentation Submission
- The provider submits an application to the insurance payer, including personal and professional details.
- Required documents may include:
- Medical license and board certifications
- Proof of education and training
- Work history and references
- Malpractice insurance coverage
- NPI (National Provider Identifier) number
- Ensuring accuracy in the initial submission helps prevent delays.
2. Primary Source Verification (PSV) & Background Checks
- The insurance company conducts a Primary Source Verification (PSV) to confirm the provider’s qualifications.
- This includes:
- Education, training, and licensing verification
- Background checks for malpractice claims, disciplinary actions, and exclusions
- Work history validation and reference checks
- Any discrepancies may lead to delays or require additional documentation.
3. Approval & Contracting
- Once verification is complete, the insurance company reviews the application for final approval.
- If approved, the provider signs a contract with the insurer.
- The provider is officially enrolled in the network and can start billing for services.
Why Alpha Core
Get Applications completed twice as fast as in-house teams
Fixed price per application — No hidden expenses
Full assistance to your billing team
Know the status of applications in real time
Dedicated account manager for your account
Real-time alerts for expiring documents

Contact Alpha Core Healthcare for Credentialing and Enrollment Services
Alpha Core Healthcare has worked with healthcare practices and organizations across the U.S., providing impeccable credentialing and enrollment services. If you need assistance completing the credentialing process with insurance companies in a timely manner, we ensure your credentialing and contracting goes as seamlessly as possible.
Countless organizations in every facet of the healthcare industry turn to Alpha Core Healthcare because we customize our medical billing services to fit our clients’ needs. From consulting to taking action on your behalf, learn more about our services when you contact us online. Or, give us a call.
Services
Contact Us
- hello@alphacorehealthcare.com
- (302) 304-8686
- 3524 Silverside Rd, Wilmington, DE 19810, United States
Copyright © 2025 Alpha Core Healthcare, All rights reserved.
